The Ecosystem of Recovery reflects the approach we are using in the Appalachian region of New York State to create broader access to and community-wide support for evidence-based and emerging best practices in opioid use disorder (OUD) treatment. This approach may be a helpful framework for other rural communities on this journey. It begins by establishing partnerships across the community to provide patients with access to treatment in their homes, emergency departments (EDs), and treatment centers. It ends with community-wide support for patients in recovery and care management integrated into primary care practices. The system is designed to increase screening, provide timely access to treatment, sustain long-term recovery, and engage primary care providers in a system of care.
In addressing substance use disorder (SUD)—as with other chronic diseases—it is important to have a system in place to support patients’ health—including elements such as prevention and screenings, acute care and long-term maintenance treatment, linkages to care, and ongoing support for patients and their families. Community engagement and commitment to addressing SUD as a chronic disease are key as well.
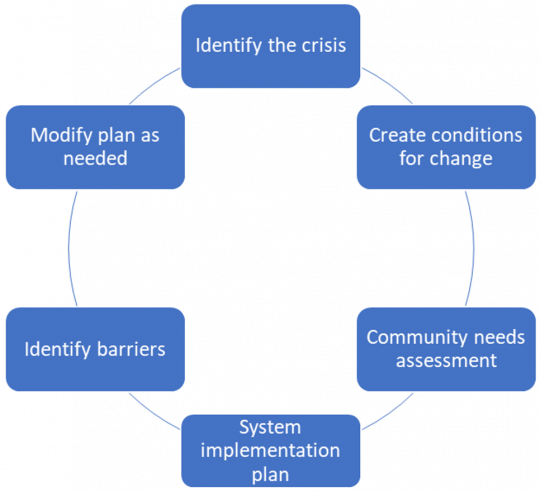
In the Ecosystem of Recovery model, a rural community builds a system1 that is geared towards local needs, working with partner organizations (which may be outside of the immediate area) and applying best practices over a period of approximately two years. This process includes the following key components:
Five Pillars
While the practices communities choose to implement may vary, it is important that—taken together—they address five priority areas or pillars:

Save Lives
- Establish programs that save lives to immediately advance community well-being and build support for creating a system of care.

Engage Community
- Champion an Ecosystem of Recovery, engaging early adopters from across organizations to build momentum towards a comprehensive, evidence-based system.2

Expand Access to Treatment
- Meet patients where they are already presenting for care and engage them in treatment, making sure the human connection to the system of care is never broken.

Screen for and Prevent SUD
- Make behavioral health screening routine during health care encounters to identify and support people at risk for SUD and normalize discussion about mental health and SUD.

Support Recovery
- Provide community-based programs and support that create opportunities for people in recovery to find healthy activities to enjoy apart from settings associated with past substance use and risky behaviors. Provide programs that assist with social determinants of health.
A wide array of programs (existing or new) can be helpful—keeping in mind that it is important to develop an initial system of care that addresses each of the five pillars and therefore does not have any major gaps. As implementation proceeds, feedback is integrated that strengthens each pillar until the program outcomes are achieving the community’s goals.
 Current vs. Future State
Current vs. Future State
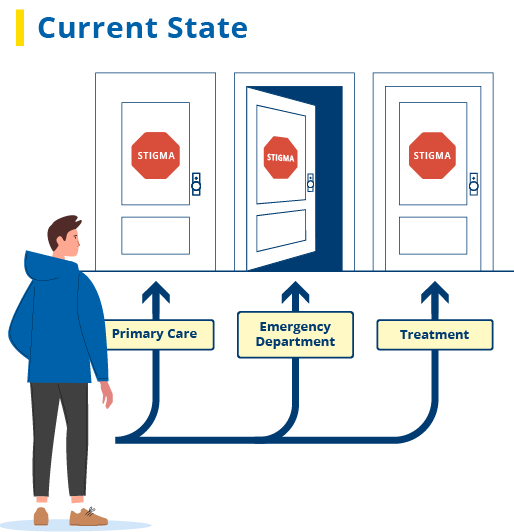
Below is an illustration of the challenges the rural communities we are partnering with in New York State initially faced.
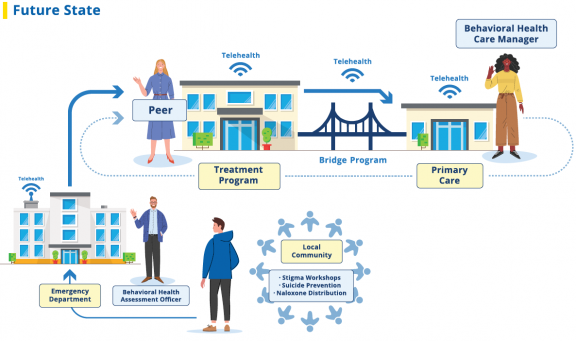
And here is an illustration of the Ecosystem of Recovery that has now been established to overcome those obstacles. That system continues to evolve to meet the needs of patients and strengthen this community effort.
Please contact Program Assistance if you would like to learn more.
References
[1] This approach to establishing a system of care is based on the work of Peter Senge, cofounder of the Academy for Systemic Change, which promotes shared understanding and leadership in solving complex problems. It requires a “network of all kinds of different learning communities [which can] really have an impact at scale, perhaps in a way that nothing else would.” Senge, P., Scharmer, O., & Winslow, D. (2013). 30 years of building learning communities. Reflections, 12(4), 40-52, p. 44.
[2] On early adopters and community engagement in relation to the overdose crisis see Quest, T. L., Merrill, J. O., Roll, J., Saxon, A. J., & Rosenblatt, R. A. (2012). Buprenorphine therapy for opioid addiction in rural Washington: The experience of the early adopters. Journal of Opioid Management, 8(1), 29–38; and Meadowcroft, D., & Whitacre, B. (2020). Community meetings on the rural opioid crisis: Setting a path forward by learning from others. Substance Abuse: Research and Treatment, 14, 1178221820920651.
February 2022