Reducing Stigma Related to SUD in Rural Care Settings
View videos and posters featuring individuals' stories and insights on reducing stigma related to SUD in care settings
Individuals with substance use disorder (SUD) who present at the emergency department (ED) are at risk for a range of poor health outcomes, including overdose and suicidal behavior.1 But an ED visit also offers a key opportunity for providers and patients to make progress toward recovery. In an ED visit, health care providers have the chance to take advantage of a “teachable moment” by engaging with patients and offering their help to initiate recovery.2 Encounters in primary care and other care settings also provide a critical opportunity to discuss treatment options and resources with patients with SUD.
Stigmatizing beliefs around SUD, however, can undermine trust in the treatment process. For people with SUD, the sense of shame that results from experiencing stigma can pose a barrier to seeking treatment, opening up about their difficulties, or returning for care, especially in small rural communities where everyone knows everyone else.3 Provider stigma can bring on a patient’s self-stigma, discouraging people with SUD from seeking care.4
UR Medicine Recovery Center of Excellence has developed a campaign that supports health care providers and staff in promoting a stigma-free treatment environment while connecting individuals and families with treatment resources.
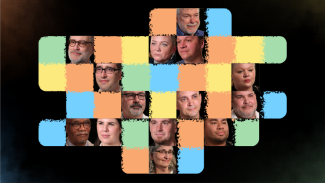
The campaign uses two well-established, evidenced-based methods for addressing stigma: 1) providing information about recovery 2) through contact with individuals in recovery.5 The center has collaborated with providers and individuals in recovery, including those from rural communities. Posters to be placed in care settings depict individuals in recovery and providers who care for patients with SUD. QR codes on the posters provide access to short videos about recovery and treatment from the individual in recovery or the provider shown on the poster.
The campaign’s strengths stem from the insights of the individuals who have been interviewed and photographed, along with using evidence-based approaches to addressing stigma.
References
[1] Bielenberg, J., Swisher, G., Lembke, A., & Haug, N. A. (2021). A systematic review of stigma interventions for providers who treat patients with substance use disorders. Journal of Substance Abuse Treatment, 131, 108486; Corrigan, P. W., & Nieweglowski, K. (2018). Stigma and the public health agenda for the opioid crisis in America. The International Journal on Drug Policy, 59, 44–49; National Academies of Sciences, Engineering, and Medicine. (2016). Ending discrimination against people with mental and substance use disorders: The evidence for stigma change. National Academies Press; Livingston, J. D., Milne, T., Fang, M. L., & Amari, E. (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction, 107(1), 39–50.
[2] Hawk, K., & D’Onofrio, G. (2018). Emergency department screening and interventions for substance use disorders. Addiction Science and Clinical Practice, 13(1).
[3] Office of National Drug Control Policy. (2020). Rural community action guide: Building stronger, healthy, drug-free rural communities.
[4] Bielenberg, J. et al. (2021).
[5] National Academies. (2016).
Updated May 2025