Rural Opioid and Direct Support Services (ROADSS)
Removing Barriers on the Road to Recovery
For people with substance use disorder (SUD), the road to recovery can be long and hard. And in rural communities, where rates of overdose mortality have increased at higher rates than in urban areas,¹ limited access to treatment makes the journey even more difficult. The Rural Opioid and Direct Support Services (ROADSS) program addresses that disparity by bringing treatment and resources that have been proven to save lives closer to home.
Studies have shown medications such as methadone reduce opioid overdose deaths. But one of the challenges in rural areas is that some patients receiving methadone must visit the location of their opioid treatment program (OTP) almost daily. The burden of long-distance travel, which can be costly and disruptive to work and family obligations, can be unmanageable.
The ROADSS program seeks to ease that burden by helping patients find the resources they need close to their community. It involves a partnership between an OTP—which may be in an urban location, like Strong Recovery in Rochester, New York—and rural organizations outside of metropolitan areas.
While there are three FDA-approved medications for opioid use disorder (OUD)—buprenorphine, methadone, and naltrexone—the ROADSS program focuses on methadone for a variety of reasons. Historically, methadone maintenance programs have demonstrated wide-ranging benefits for people with OUD and the communities in which they live, such as reducing deaths among people with OUD by approximately 50%, HIV and hepatitis infections, and drug-related crime. Patients in methadone programs have shown improvement in social functioning and tend to stay in rehabilitation programs longer.² Research also indicates methadone is effective and safe during pregnancy.³
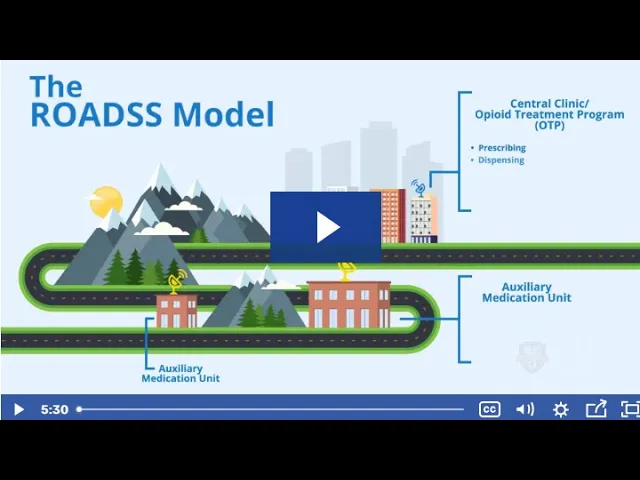
In the ROADSS model, the OTP serves as a central location offering a range of services, including individual and group counseling, prescribing, and methadone dispensing. Auxiliary sites in rural areas, meanwhile, focus on dispensing. Since dosing is more frequent than other aspects of methadone maintenance treatment, these auxiliary sites allow patients in rural communities to receive their medication without having to travel to a distant OTP. In a sense, they expand the dispensing room of the central OTP. The auxiliary sites utilize telehealth to consult with the central OTP and to facilitate patients’ access to other services at the clinic. By using telehealth for individual and family counseling, for instance, the auxiliary sites can further reduce travel demands for patients in rural communities. In addition, auxiliary sites in the ROADSS program are equipped with broadband internet that patients have the option to use.
The ROADSS model takes a regional approach that addresses the specific challenges of methadone delivery. It provides financial and operational guidance to organizations, helps them navigate federal and state regulations, and provides resources to apply in achieving community support.
References
[1] Mack, K. A., Jones, C. M., & Ballesteros, M. F. (2017). Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas—United States. American Journal of Transplantation, 17(12), 3241-3252.
[2] Schuckit, M. A. (2016). Treatment of opioid-use disorders. New England Journal of Medicine, 375(4), 357-368.
[3] National Academies of Sciences, Engineering, and Medicine. (2019). Medications for opioid use disorder save lives. National Academies Press, p. 70.


